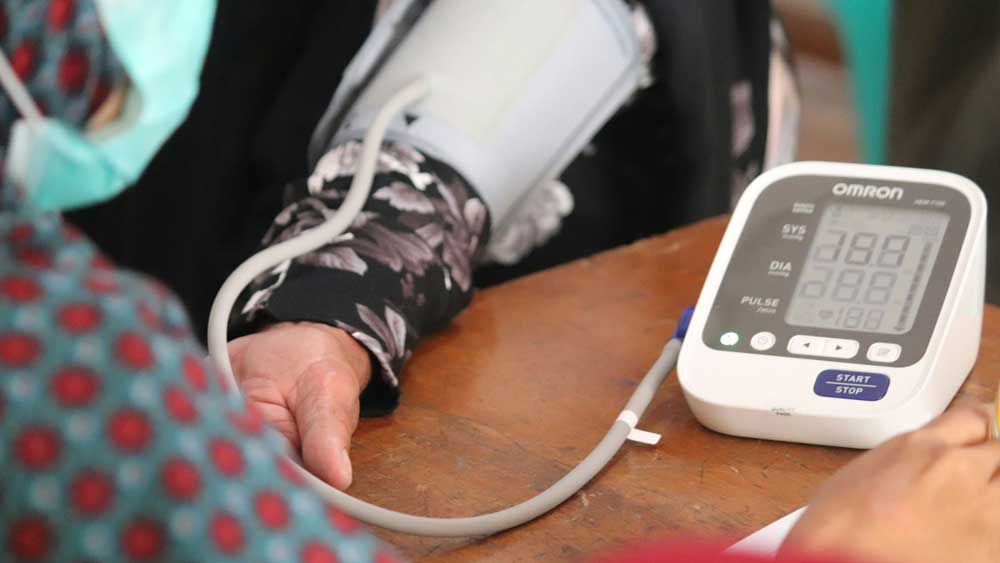
Photo by Mufid Majnun on Unsplash
Compliance with industry regulations and standards is a fundamental part of medtech. Without proper medical device compliance, companies risk patient harm, litigation, and reputational damage.
|
ADVERTISEMENT |
Fortunately, compliance with medical device regulations and standards is not an impossible task. A companywide emphasis on quality, along with the right tools for the job, can ensure that you stay compliant and produce the safest, most effective medical devices possible.
Here’s what you need to know about compliance in the medtech industry.
What is medical device compliance?
Medical device compliance refers to the way a company meets the requirements of all applicable regulations and standards. Medical device compliance should begin during design and development, and must be maintained throughout the entire life cycle of the device.
…
Add new comment